To guide clinicians in the selection of antithrombotic therapy for the prevention of ischemic stroke and arterial thromboembolism in patients with atrial fibrillation.
Atrial fibrillation (AF) is the most common pathologic arrhythmia and increases in prevalence with increasing age (prevalence of 10-15% in patients who are ≥80 years). The most devastating complication of AF is arterial embolism of a left atrial thrombus resulting in ischemic stroke, peripheral limb ischemia, or other end organ damage. AF is associated with a 3- to 6-fold increased risk of stroke or non-central nervous system (CNS) systemic embolism. Furthermore, ischemic strokes in patients with AF are larger and more frequently associated with death and disability than strokes that occur in the absence of AF. Therefore, stroke prevention is a critical part of AF treatment.
The risk of arterial thromboembolism can be significantly reduced with anticoagulant therapy (warfarin, apixaban, dabigatran, edoxaban or rivaroxaban) and, to a much lesser extent, with antiplatelet therapy. Selection of antithrombotic therapy should be guided by assessment of presumed thrombotic risk, assessment of presumed bleeding risk on antithrombotic therapy and patient preference.
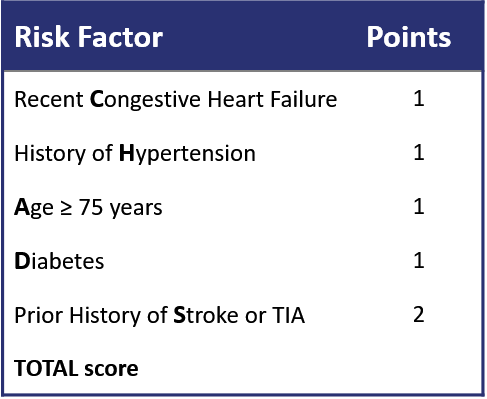
Thrombotic Risk: Prognostic models incorporating patient age and co-morbidities provide validated estimates of the annual risk for thromboembolism without anticoagulant therapy. These models were developed for patients with non-valvular AF, which refers to AF occurring in the absence of a mechanical heart valve or rheumatic heart disease with severe mitral stenosis or regurgitation. The most frequently used score is the CHADS2 score (see Table 1). A modification of this score is the CHA2DS2-VASc score which incorporates age 65-75 years (1 point), age ≥75 (2 points), female sex (1 point), and presence of vascular disease (1 point). These risk calculators are available on the Thrombosis Canada website [http://thrombosiscanada.ca/?page_id=502]. In general, in patients with a CHADS2 score or a CHA2DS2-VASc score ≥1, the risk of arterial thromboembolism (and resulting morbidity/mortality) without anticoagulation outweighs the risk of bleeding from anticoagulants.
Table 1: CHADS2 Score for Assessment of Risk of Stroke or Systemic Embolism in Patients with Non-Valvular AF
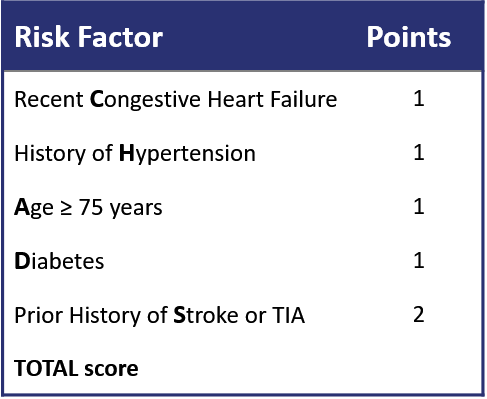
The Canadian Cardiovascular Society and this guide use the “CHADS-65”scoring system as the basis for its recommendations (see Recommendations and Figure 1).
Bleeding Risk: Bleeding risk should also be assessed in all patients. However, in most cases, bleeding risk should not preclude the use of anticoagulant therapy. The risk-benefit ratio almost always favours anticoagulation unless the risks for bleeding are very high and the risk of thromboembolism is very low. Patients at increased risk for bleeding, typically, are also those who will benefit the most from anticoagulation to prevent stroke, and attempts should be made to modify bleeding risk factors (i.e. NSAID or alcohol use, frequent falls). There are prognostic models for the estimation of bleeding risk in patients with AF on warfarin therapy (e.g. HAS-BLED, available on Thrombosis Canada website, http://thrombosiscanada.ca/?page_id=502), which can help to identify potentially reversible risk factors for bleeding.
Anticoagulants: Warfarin (with target INR of 2-3) was the anticoagulant of choice for the prevention of stroke in patients with AF for many years. The newer direct oral anticoagulants (DOACs), which consist of apixaban, dabigatran, edoxaban, and rivaroxaban are used increasingly for this indication, and are suggested in preference to warfarin in the Canadian Cardiovascular Society’s guidelines for the management of AF. Large randomized trials indicate non-inferior or superior efficacy and safety compared with warfarin. Practical advantages of DOACs (also known as NOACs, non-vitamin K oral anticoagulants) over warfarin include fixed, once- or twice-daily oral dosing without the need for routine coagulation monitoring, few known or defined drug interactions, no known food interactions, and lower risks of intracranial bleeding. Potential disadvantages include lack of readily available reversal agents for rivaroxaban, apixaban, and edoxaban in case of major bleeding (although andexanet alfa has been licensed for this indication in the United States) and varying degrees of renal elimination requiring dose adjustment in patients with renal insufficiency (see Table 2). An antidote for dabigatran (idaruzicumab) is approved by Health Canada and is widely available. Patients taking DOACs require periodic monitoring of renal function. Like warfarin, DOACs increase the risk for bleeding.
There have been no head-to-head clinical trials comparing one DOAC with another and there is no evidence to suggest superior efficacy or safety of one agent over another. Practical issues regarding the everyday use of DOACs are addressed in the Clinical Guide: NOACs/DOACs: Comparison and Frequently Asked Questions.
Table 2: DOAC drug dosing for patients with AF according to renal function†


Antiplatelet agents:
In patients with AF at low risk of stroke, who decline oral anticoagulation, or in whom oral anticoagulation is considered contraindicated due to bleeding risk, low dose aspirin (80-100 mg/day) may be considered. However, aspirin provides less protection than an anticoagulant and increases bleeding risk.
See Figure 1 below (from the Canadian Cardiovascular Society Update of AF guidelines).
For patients age <65 with non-valvular AF at low risk of stroke (CHADS2 score = 0) and no other risk factors, no antithrombotic therapy is needed. In patients age <65 who have coronary artery or other vascular disease, ASA 81 mg daily should be used.
For patients with non-valvular AF age >65 or <65 with any of the CHADS2 risk factors, anticoagulation with a DOAC or warfarin (target INR 2.0-3.0) is indicated. The Canadian Cardiovascular Society states that a DOAC is the preferred choice. For patients who are unsuitable for or who decline anticoagulants, ASA 81 mg daily is suggested.

Special considerations:
Patients with AF and valvular heart disease (severe mitral stenosis, mechanical heart valves) are at significantly increased risk for ischemic stroke, and warfarin is recommended for this indication. Treatment with a DOAC is not recommended in these patients with AF and these drugs are not approved for this use.
In patients with coronary artery disease, antithrombotic management should be individualized.
Andrade JG, et al. 2018 focused update of the Canadian Cardiovascular Society Guidelines for the management of atrial fibrillation. Can J Card 2018;34:1371-1392.
Connolly SJ, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361(12):1139–1151.
Gage BF, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 2001;285(22):2864-2870.
Granger CB, et al. Apixaban versus warfarin in patients with atrial fibrillation. New Engl J Med 2011;365(11):981–993.
Lip GYH, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on Atrial Fibrillation. Chest 2010;137(2):263-272.
Patel MR, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. New Engl J Med 2011;365(10):883–891.
Pisters R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 2010:138(5);1093-1100.
Date of Version: 14Jan2020
Please note that the information contained herein is not to be interpreted as an alternative to medical advice from your doctor or other professional healthcare provider. If you have any specific questions about any medical matter, you should consult your doctor or other professional healthcare providers, and as such you should never delay seeking medical advice, disregard medical advice or discontinue medical treatment because of the information contained herein.